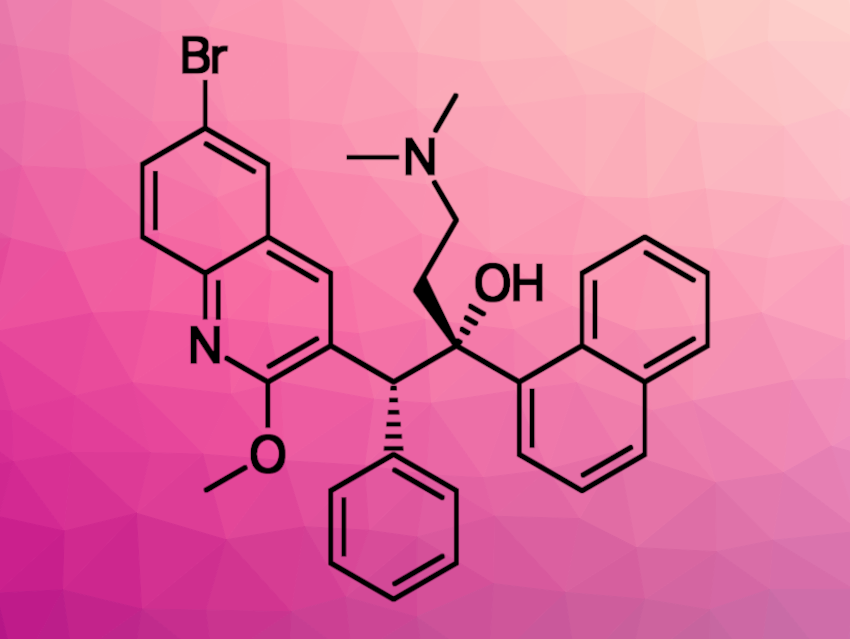
Tuberculosis (TB) is an important global health concern. In particular, an increase in infections with multidrug-resistant Mycobacterium tuberculosis strains is concerning. To improve tuberculosis treatment and reduce side effects, delivering drugs directly to the lungs in high local doses could be useful. Nanocarrier-based drug delivery is a promising approach to this. Bedaquiline (BDQ, pictured) and 1,3-benzothiazin-4-ones (BTZs), for example, are two types of drugs that can be used to treat multidrug-resistant TB strains. However, they are lipophilic and, thus, difficult to transport in aqueous systems. Amorphous drug nanoparticles could be promising for the delivery of such poorly soluble antibiotics to the lungs.
Lea Ann Dailey, University of Vienna, Austria, Ulrich E. Schaible, Research Center Borstel, Leibniz Lung Center, and German Center for Infection Research (DZIF), both Borstel, Germany, Claus Feldmann, Karlsruhe Institute of Technology (KIT), Germany, and colleagues have prepared high-dose, amorphous nanoparticles of bedaquiline and 1,3-benzothiazin-4-one 043. The team used a solvent-antisolvent technique: A concentrated “solvent” solution of BDQ/BTZ in dimethylsulfoxide (DMSO) was injected into water as the “antisolvent”. They also used a surfactant to stabilize the nanoparticles, i.e., a mixture of monododecylphosphate and α-tocopherolphosphate for BDQ and sodium dodecyl sulfate for BTZ. The resulting particles have mean diameters of ca. 60 nm for BDQ) and ca. 62 nm for BTZ.
The nanoparticles have high drug loads, and the team found that they were effective against Mycobacterium tuberculosis both in vitro and in a mouse model. For BTZ, the nanoparticles were more effective in vivo than the freely dissolved drug. According to the researchers, using amorphous drug nanoparticles of poorly soluble antibiotics for inhalation therapy could overcome existing limitations that are associated with inhaled antibiotics, and further development of this strategy could improve tuberculosis treatment.
- Amorphous Drug Nanoparticles for Inhalation Therapy of Multidrug-Resistant Tuberculosis,
David Rudolph, Natalja Redinger, Katharina Schwarz, Feng Li, Gabriela Hädrich, Michaela Cohrs, Lea Ann Dailey, Ulrich E. Schaible, Claus Feldmann,
ACS Nano 2023.
https://doi.org/10.1021/acsnano.3c01664