Breast milk remains the “gold standard” of baby nutrition: numerous investigations in recent decades have supported its positive effects on the development of nursing infants. As far back as the early 19th century, pediatricians determined that the mortality of infants fed with breast milk was significantly lower than that of those who received no breast milk [1].
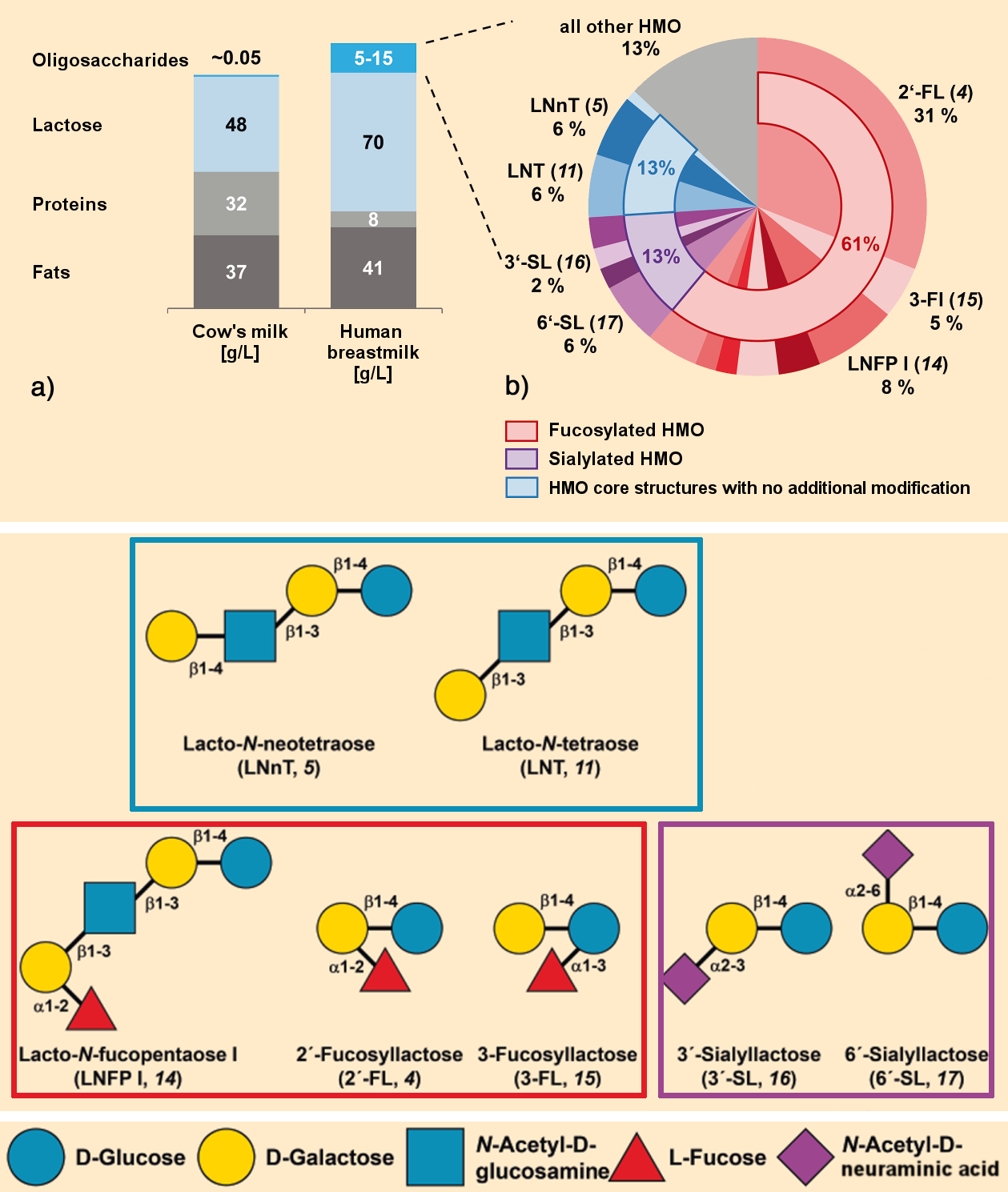
In addition to water, lactose (which delivers energy), fats, and proteins, breast milk contains a number of other important components needed for the healthy development of an infant (see Fig. 1). One of these classes of biologically active substances is comprised of the human milk oligosaccharides (HMO) (see Fig. 2). HMO are not digested by the infant; instead, they feed their gut bacteria. These provide energy to the baby, train its immune system, and fend off pathogens.
Understanding the structures, synthesis, and function of these over 200 different HMO molecules is a hot topic. The first infant formulas that include individual HMOs to more closely match the composition of breast milk are already on the market. In this article, we will take a look at the history of HMO chemistry and the latest developments in this area.
1. Sugar Chemistry
.jpg) Oligosaccharides are carbohydrates consisting of three to ten monosaccharide units bound together through glycosidic bonds. The myriad ways in which these monomers can be bound together lead to an enormous diversity of oligosaccharides (see Infobox 1).
Oligosaccharides are carbohydrates consisting of three to ten monosaccharide units bound together through glycosidic bonds. The myriad ways in which these monomers can be bound together lead to an enormous diversity of oligosaccharides (see Infobox 1).
In the context of human nutrition, we often associate sugars with poor nutrition or obesity because industrialized societies have an overabundance of sugar-containing, energy-rich foods available. In addition to acting as a source of energy, sugar plays many important roles in the body.
For humans, the subset of sugars found in food known as functional oligosaccharides is very important. For example, they may boost our health by acting as prebiotics and supporting the growth of beneficial bacteria in the large intestine. Not every important sugar is absorbed from food, however. Humans are also capable of producing functional oligosaccharides in their bodies. One interesting example of this is breast milk.
2. Breast Milk
Lactation through the mammary glands by females, also called nursing, is the characteristic that gives the entire class of animals known as mammals its name.
2.1. Components of Breast Milk
Milk is a highly complex mixture of water and nutrients with a complex production process. It primarily consists of lactose, fats, oligosaccharides, and proteins (see Fig. 1). In humans, the amount of energy required daily for the production of milk is about 500 kcal, which is at the same order of magnitude as the energy required by the brain.
 |
|
Figure 1. Composition of human breast milk compared with cow’s milk [2]. |
There are many qualitative differences between the breast milks produced by different species of mammal: The milk of primates and marsupials is dominated by carbohydrates; marine mammals produce milk that is very high in fat; and species with offspring that must grow fast, such as reindeer, have milk that is very protein-rich.
Human breast milk has a functional oligosaccharide content that is 100 to 300 times higher than cow’s milk (see Fig. 1). For this reason alone, cow’s milk is not an equivalent substitute for human milk.
Breast milk provides children with a wide range of biologically active components, such as hormones, growth factors, immunoglobulins, cytokines (messenger molecules that regulate growth and the immune system), antimicrobial peptides, enzymes, a large number of pre- and probiotics, and functional oligosaccharides.
Human breast milk contains 5–15 g/L HMOs (see Fig. 2) [3]. As appropriate to the development of the growing child, early or first milk (colostrum) contains a higher proportion of HMO than breast milk that is produced later. In addition, the HMO content and HMO composition vary throughout the day, as well as based on the age and the ethnic, physiological, and genetic characteristics of the mother, such as her blood type [3,4].
.jpg) |
|
Figure 2. General structure of human milk oligosaccharides (HMO) [9]. |
Breast milk is optimally tuned to the requirements of the child. For this reason, breastfeeding is a “simple, inexpensive primary prevention measure”, to ensure the healthy development of children. The WHO recommends exclusively breastfeeding infants for the first six months. In addition to appropriate supplemental food, the WHO further recommends that children should continue nursing until they are two years old. According to figures from the WHO for 2017/2018, only 40 % of all babies (0–6 months) are exclusively breastfed and 60 % are partially breastfed [5,6].
For infants that cannot be breastfed for a variety of reasons, a number of alternatives have been found over the centuries. Examples include the use of wet nurses or bottle feeding with breast milk, and later with industrially produced infant formulas.
2.2. When Are Alternatives to Nursing Needed? A Historical Outline
Medical Reasons
In the days of high maternal mortality, infants whose mothers had died were fed by wet nurses. Until bottle feeding was introduced in the 19th century, the wet nurse was the only alternative to nursing for feeding a baby.
Other medical reasons for using a wet nurse or bottle feeding are an insufficient maternal milk supply (hypo- or agalactia) or the occurrence of mastitis.
Societal Reasons
In addition to these medical issues, there were and continue to be societal reasons for which infants cannot be breastfed by their mothers. In the Renaissance, it was unusual for women of the aristocracy to breastfeed. Instead, this task was given over to a wet nurse.
Later, nursing became rarer in less affluent levels of society as well, though less for reasons of convenience and more due to economic necessity. In a merchant’s household, for example, it made more sense economically to pay a wet nurse than to hire temporary personnel to compensate for the lost labor of the nursing mother. As the Industrial Revolution made the employment of women a necessity for the economic survival of the family, it became nearly impossible for mothers to nurse their own infants. Babies were handed off to wet nurses, whose economic circumstances were even more precarious than those of the mothers.
In the 19th century, the first products for feeding babies intended as alternatives to breastfeeding or wet nurses came on the market. In 1865, German scientist Justus von Liebig (1803–1870) patented a baby formula he had developed based on cow’s milk, wheat flour, and potassium carbonate. This was sold as a powder at the time [1]. The introduction of food preservation as well as the baby bottle and nipple eventually led to the spread of bottle feeding in many industrialized nations at the beginning of the 20th century.
The Current Situation
Today, a variety of industrially prepared early-infant and follow-up foods (called formula foods) are available. Their compositions are based on the latest research results and the recommendations of pediatricians and nutritionists [7]. However, breastfeeding remains the “gold standard” for feeding infants. For this reason, society and governments are asked to promote and allow breastfeeding through legal frameworks.
So-called “bottle” babies consume infant starter and follow-up foods based on cow, goat, or soymilk that differ greatly from human breast milk with regard to HMO content. The composition of this, often sole, source of nutrition in the first months of life is very important, since this is a phase marked by rapid growth and enormous development that is never matched later in life. The requirements for the composition and marketing of formula are, thus, strictly regulated.
The better our understanding of the composition and importance of breast milk has grown over time, the more effort has been made to make the composition of formula more similar to that of breast milk, through the selection of proteins, the addition of long-chain polyunsaturated fatty acids, or the inclusion of HMO.
The baby food market was estimated to be worth 50 billion US dollars in 2017, with an expected potential to reach 69 billion US dollars by 2023 [8]. The expansion of the middle class in developing nations and the BRICS nations (Brazil, Russia, India, China, South Africa) increases the demand for significantly improved infant starter and follow-up formulas. This market potential is an important driving force for research into HMO and their industrial production.
The first infant formulas with added HMOs are already on the market: “Similac®” contains 2′-fucosyllactose (2′-FL, 4) (see Fig. 1) and has been sold by the Abbott corporation in the USA since 2016. Since 2017, Nestlé of Vevey, Switzerland, has sold “NAN®“, an infant formula containing 2’FL (4) and lacto-N-neotetraose (LNnT, 5), in Spain.
Companies that produce HMOs in industrial quantities include BASF SE (Germany), Jennewein Biotechnology GmbH (Germany), Glycom A/S (Denmark), DuPont Nutrition & Health (USA), and Friesland Campina Domo B.V. (The Netherlands) [9].
References
[1] C. Kunz, Historical Aspects of Human Milk Oligosaccharides, Adv. Nutr. 2012, 3, 430S–439S. https://doi.org/10.3945/an.111.001776
[2] K. Bych et al., Production of HMOs using microbial hosts – from cell engineering to large scale production, Curr. Opin. Biotechnol. 2019, 56, 130–137. https://doi.org/10.1016/j.copbio.2018.11.003
[3] L. Bode, Human milk oligosaccharides: every baby needs a sugar mama, Glycobiology 2012, 22, 1147–1162. https://doi.org/10.1093/glycob/cws074
[4] C. Kunz et al., in Food Oligosaccharides: Production, Analysis and Bioactivity, John Wiley & Sons, Hoboken, NJ, USA, 2014. ISBN: 978-1-118-42649-4
[5] WHO, UNICEF, Global breastfeeding scorecard, Tracking progress for breastfeeding policies and programmes, UNICEF New York, USA, and WHO Genf, Switzerland, 2017.
[6] WHO, UNICEF, IBFAN, Marketing of breast-milk substitutes: national implementation of the international code. Status Report 2018, UNICEF New York, USA, and WHO Genf, Switzerland, 2018.
[7] B. Koletzko et al., Global standard for the composition of infant formula: recommendations of an ESPGHAN coordinated international expert group, J. Pediatr. Gastroenterol. Nutr. 2005, 41, 584–599. https://doi.org/10.1097/01.mpg.0000187817.38836.42
[8] T. Nguyen, Synthesizing mothers’ milk – Scientists are seeking ways to make beneficial but elusive sugars found in breast milk, Chem. Eng. News 2018, 96, 26.
[9] G. A. Sprenger et al., Production of human milk oligosaccharides by enzymatic and whole-cell microbial biotransformations, J. Biotech. 2017, 258, 79–91. https://doi.org/10.1016/j.jbiotec.2017.07.030
The article has been published in German as:
- Mehr als 200 gute Gründe für das Stillen,
Michael Breuer, Melanie Weingarten,
Chem. unserer Zeit 2019, 53, 94–104.
https://doi.org/10.1002/ciuz.201900030
and was translated by Caroll Pohl-Ferry.
Nursing, Gut Bacteria, and the Immune System – Part 2
What are human milk oligosaccharides (HMO)?
Nursing, Gut Bacteria, and the Immune System – Part 3
How are human milk oligosaccharides (HMO) synthesized?
Nursing, Gut Bacteria, and the Immune System – Part 4
Which effects do human milk oligosaccharides (HMO) have?
See similar articles published on ChemistryViews.org