Forensic sciences are a highly diverse field. Forensic toxicology, for example, can play an important role. This article provides a look behind the scenes at two representative case reports that illustrate the different approaches followed in the field of forensic toxicology.
1. What is Forensic Medicine?
Forensic medicine is primarily concerned with cases in which the victim has died of indeterminate causes, according to a public prosecutor. Forensic medicine and forensic toxicology play a special role in finding the cause of death.
If the cause of death is unknown, the physician who performed the autopsy and the state prosecutor refer the body to the forensic pathologist. Usually working with an autopsy assistant, the forensic pathologist examines the corpse in minute detail and takes samples.
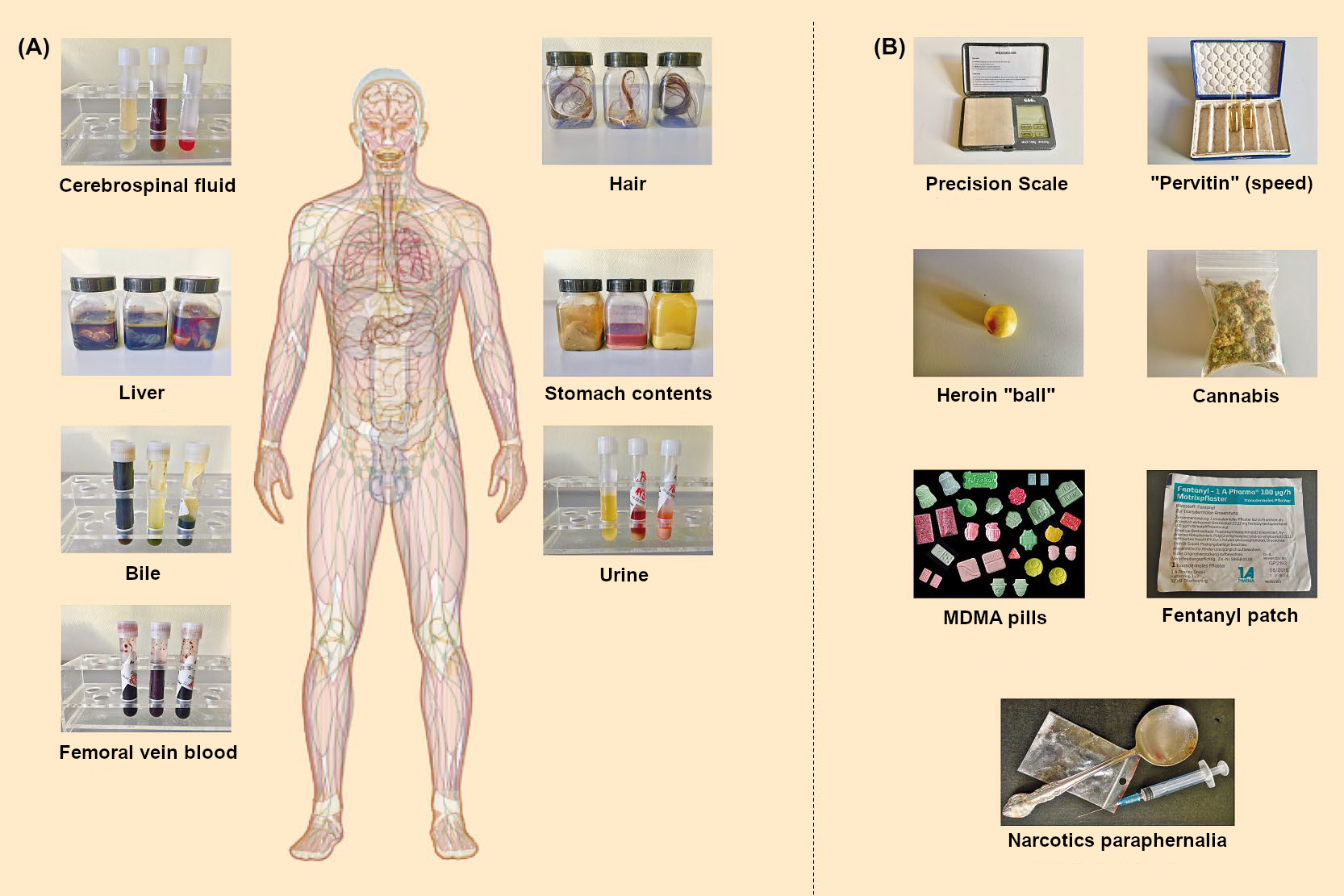
The autopsy is followed by a toxicological analysis, which attempts to determine if a third party was responsible for the death. The toxicological result gives information about whether the victim was poisoned or poisoned themselves. This finding is recorded in a separate report. The toxicological examination involves testing samples of the corpse—usually blood from the femoral vein and urine, in some cases also hair—for toxins. Sometimes, further analyses are carried out on the gall bladder and stomach contents to better determine if poisoning occurred.
In this article, we invite you to a look behind the scenes of forensic medicine. Learn about our work from the outside with your eyes wide open before you possibly see it from the inside.
 |
|
Figure. Autopsy room. |
2. Drug Consumption
In Berlin, Germany, over 30,000 people die every year [1]. The causes of death vary greatly. They include heart attacks, terminal care, hanging, and polytrauma, as well as a golden shot of heroin or an overdose of cocaine or another drug, just to name a few. Annually, about 150 people die from drug consumption.
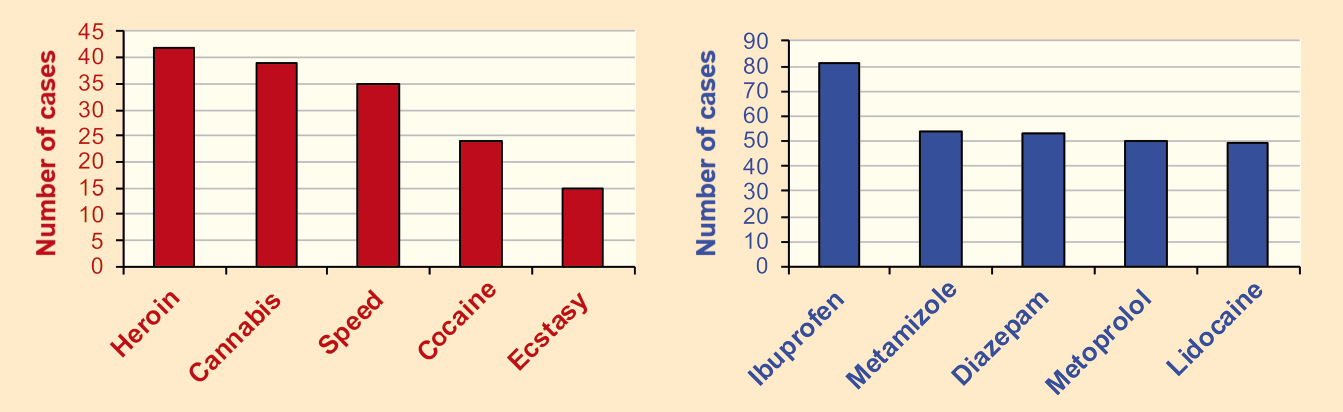
 In the year 2016, the State Institute of Forensic and Social Medicine primarily detected heroin, cannabis, speed, cocaine, and ecstasy in samples of femoral vein blood. Commonly found medications were ibuprofen, metamizole, diazepam, metoprolol, and lidocaine (see Fig. 1 and Info Box 1). However, these substances are not always the cause of death. For example, death may be caused by the consumption of multiple drugs or medications.
In the year 2016, the State Institute of Forensic and Social Medicine primarily detected heroin, cannabis, speed, cocaine, and ecstasy in samples of femoral vein blood. Commonly found medications were ibuprofen, metamizole, diazepam, metoprolol, and lidocaine (see Fig. 1 and Info Box 1). However, these substances are not always the cause of death. For example, death may be caused by the consumption of multiple drugs or medications.
 |
|
Figure 1. Drugs and medications detected in the femoral vein blood of corpses in the city of Berlin, Germany, at the State Institute of Forensic and Social Medicine in 2016. |
3. In the Autopsy Room
Every year, 2,000—2,2000 corpses are autopsied in Berlin—about half of those at the State Institute of Forensic and Social Medicine, the other half at the Institute of Forensic Medicine at the Charité University Hospital in Berlin.
3.1 What Is an Autopsy?
An autopsy is the opening of a corpse to determine the cause of death and the exact circumstances of the death. It is ordered by the prosecution and consists of external and internal examinations. It usually begins with an outer examination of the corpse. Basic information like weight, height, skin color, and overall condition of the body are recorded, as well as scars, moles, and possible wounds. Signs of trauma are particularly significant. Physical features of the death are also noted, such as the amount and location of lividity.
Lividity is a purple-red to blue-gray discoloration of the skin that results from the sinking of blood in the blood vessels due to gravity. Lividity begins to appear 20–30 minutes after blood circulation stops.
After the external examination of the body, the internal dissection begins. In this part of the autopsy, the corpse is examined for pre-existing disease, acute disease, and general signs of death. Evidence may include liquid blood from the corpse, a full bladder, blood stasis in organs, swelling of the brain, and edema of the lungs. Specific characteristics allow the physician to decide which diseases or unnatural causes could have led to the death.
3.2 Samples from the Corpse
In addition to the inner and outer examinations of the corpse, a complete set of samples is taken from the body to test for toxicological effects. These include urine, blood from the femoral vein and the heart, bile, stomach contents, liver, cerebrospinal fluid, fluid from the vitreous humor, and hair from the head (see Fig. 2). In rare cases, blood from hematomas and samples of lung tissue are collected. Additionally, all evidence found at the scene of death is included, such as precision scales, vials, balls containing individual heroin doses, parts of cannabis plants, patches, narcotics paraphernalia, and, of course, pills of all colors, shapes, and types. The latter are usually not found on the corpse, but at the location where it was found.
 |
|
Figure 2. Biological (A) and nonbiological (B) evidence for toxicological analysis. |
In the case of heavily decomposed corpses, not all samples can be obtained, because the corpse has already changed too much. Often, only muscle, liver, and decomposition fluid can be obtained and tested for poisoning.
3.3 Beginning the Toxicological Analysis
If the medical examiner cannot rule out toxicological influence after the autopsy, a toxicological analysis is ordered. This involves a systematic toxicological analysis (STA) to detect toxins. The toxin could be a gas, liquid, or solid. These could be organic or inorganic. Modern poisonings are most often detected by using STA.
 Systematic toxicological analysis is a core concept in toxicology and includes group tests, as used in immunoassays (see Info Box 2), special analyses, such as CO- and CN detection after a fire, or alcohol detection and the detection of volatile organic compounds using headspace solid-phase microextraction gas chromatography–mass spectrometry (Headspace-SPME-GC/MS). Additionally, it includes the detection of metals with atomic absorption spectroscopy (AAS) and ICP-MS (inductively coupled plasma mass spectrometry), as well as the detection of organic toxins with LC/MS (liquid chromatography coupled to mass spectrometry), GC/MS (gas chromatography coupled to mass spectrometry) and LC/DAD (liquid chromatography with photodiode array detection) [2,3].
Systematic toxicological analysis is a core concept in toxicology and includes group tests, as used in immunoassays (see Info Box 2), special analyses, such as CO- and CN detection after a fire, or alcohol detection and the detection of volatile organic compounds using headspace solid-phase microextraction gas chromatography–mass spectrometry (Headspace-SPME-GC/MS). Additionally, it includes the detection of metals with atomic absorption spectroscopy (AAS) and ICP-MS (inductively coupled plasma mass spectrometry), as well as the detection of organic toxins with LC/MS (liquid chromatography coupled to mass spectrometry), GC/MS (gas chromatography coupled to mass spectrometry) and LC/DAD (liquid chromatography with photodiode array detection) [2,3].
The analytical methods employed are very versatile and range from simple photometric analysis to chromatographic systems coupled to either selective or universal detectors.
3.4 Tracking Down Targets that Might Have Induced Death
3.4.1 Detection
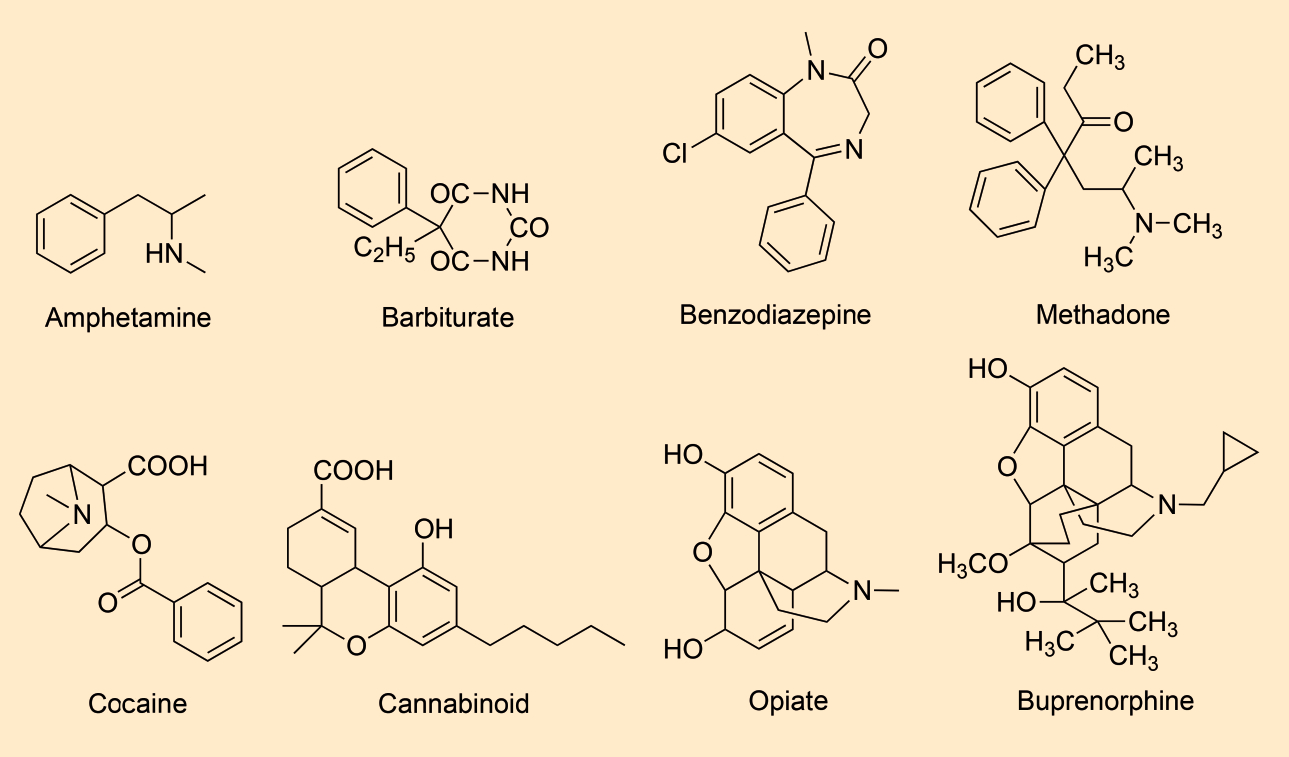
At the beginning of the systematic analysis, a urine sample is analyzed for certain groups of substances or individual substances using a variety of immunochemical methods. These substances usually include amphetamines, barbiturates, benzodiazepines, opiates, cocaine metabolites, cannabinoids, methadone, and buprenorphine (see Fig. 3 and Info Box 2).
 |
|
Figure 3. Individual substances and substance groups currently detected immunochemically in blood and urine samples from corpses, illustrated with corresponding examples: amphetamines (e.g., methamphetamine), barbiturates (e.g., phenobarbital), benzodiazepines (e.g., diazepam), cocaine metabolites (e.g., benzoylecgonine), cannabinoids (e.g., THC-COOH), opiates (e.g., morphine), buprenorphine, and methadone. |
For detecting potential toxins, urine is the matrix (test object) of choice. However, if the bladder is empty at the time of autopsy, blood from the heart is subjected to immunochemical analysis instead, although cannabinoids, certain benzodiazepines, and buprenorphine are difficult to detect in this matrix.
 “New psychoactive substances” are difficult to detect in urine and blood because this market changes so rapidly that only few screening tests exist. New psychoactive substances like piperazine, phencyclidine, phenethylamine, synthetic cathinones, synthetic cannabinoids, and synthetic opioids, are preferentially detected using mass spectrometric techniques involving a liquid chromatograph and a high-resolution mass spectrometer (see Info Box 3). The advantage of this method is that these previously unknown substances are easier to identify.
“New psychoactive substances” are difficult to detect in urine and blood because this market changes so rapidly that only few screening tests exist. New psychoactive substances like piperazine, phencyclidine, phenethylamine, synthetic cathinones, synthetic cannabinoids, and synthetic opioids, are preferentially detected using mass spectrometric techniques involving a liquid chromatograph and a high-resolution mass spectrometer (see Info Box 3). The advantage of this method is that these previously unknown substances are easier to identify.
3.4.2 Confirmational Analysis
If the amount of one of the abovementioned groups or substances (see Fig. 3) is found to be above a defined limit, the next step is a confirmational analysis to determine the identity of the toxin. This is usually carried out with a gas chromatograph that is coupled to a mass spectrometer. In the first step of a GC/MS analysis, the sample is vaporized. The individual components are then separated. The boiling point of each substance determines if a substance elutes earlier or later to be detected at the exit of the column.
Usually, the sample is derivatized (acetylated or methylated) before this analysis to reduce the boiling point of the less volatile substances in the sample. This method is very frequently used in forensic toxicology laboratories because it is very robust, and results can easily be shared between different laboratories. For example, if one laboratory has a mass spectrum for a new drug or medication, this spectrum can easily be shared with other forensic toxicology labs for comparison.
3.4.2 Evaluation
Various commercially available and public mass spectrum libraries are used for the interpretation of GC/MS spectra. These enable relatively fast matching of the sample spectrum with one from the library. One of the most comprehensive libraries of mass spectra in the field of forensic toxicology is the Maurer-Pfleger-Weber library. It includes 10,430 mass spectra of potentially toxic substances and 7,800 spectra of metabolites [4]. Another library of spectra is the Rösner library of “designer drugs”, which includes 25,114 spectra and is especially helpful in detecting new psychoactive substances [5]. In addition, there are various publicly available mass spectrum libraries, such as the Cayman library [6] and the SWGDRUG library [7].
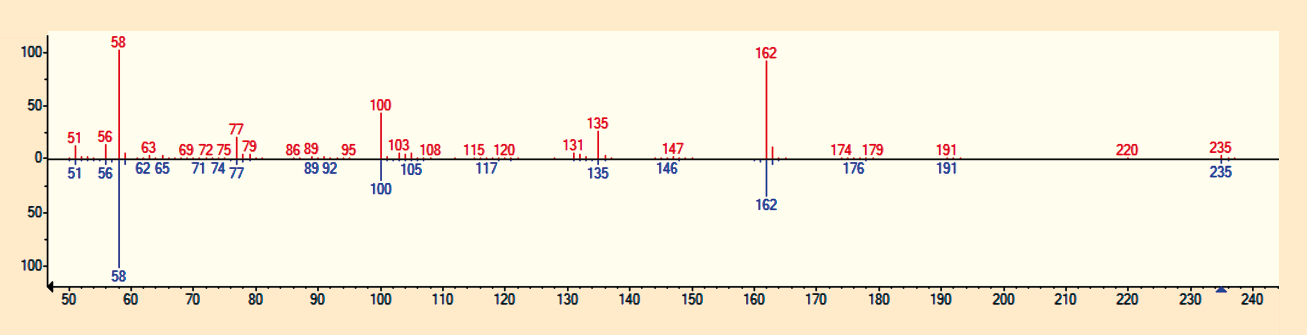
If a sufficient number of mass fragments and intensity ratios from the sample match those of a library spectrum, the software assigns a high match factor. For a successful match, the match factor between the sample spectrum and the library spectrum should be higher than 500 and the retention time must match the standard (see Fig. 4).
 |
|
Figure 4. Comparison of a recorded mass spectrum with a library spectrum to detect poisoning. The match factor is 872 and the reverse match factor 878 for acetylated MDMA. |
If no standard reference measurement has yet been made because the reference substance is difficult to obtain commercially or costs a fortune, previous cases of poisoning are used. These either come from the laboratory carrying out the current test or from other forensic toxicology laboratories. The newly recorded profile is then compared with the old profile.
More recent efforts couple a liquid chromatograph with a high-resolution mass spectrometer (Orbitrap or QToF). The mass spectrum libraries for these methods are not yet as comprehensive as those for GC/MS analysis, so these techniques are still in development. It should also be mentioned that the MS/MS spectra definitely differ from one lab to another and cannot be as easily shared.
References
[1] Anzahl der Sterbefälle in Berlin von 1991 bis 2020 (in German), de.statista.com. (accessed March 2018)
[2] H. H. Maurer, Systematic toxicological analysis of drugs and their metabolites by gas chromatography–mass spectrometry, J. Chromatogr. 1992, 580, 3–41. https://doi.org/10.1016/0378-4347(92)80526-v
[3] S. Broecker et al., Development and practical application of a library of CID accurate mass spectra of more than 2,500 toxic compounds for systematic toxicological analysis by LC–QTOF-MS with data-dependent acquisition, Anal. Bioanal. Chem. 2011, 400, 101–117. https://doi.org/10.1007/s00216-010-4450-9
[4] Hans H. Maurer et al., Mass Spectral and GC Data. www.mswil.com. (accessed December 2021).
[5] Peter Rösner, Mass Spectra of Designer Drugs 2021, Wiley-VCH, Weinheim, 2021. ISBN: 978-3-527-35006-3
[6] Cayman Spectral Library, www.caymanchem.com. (accessed December 2021)
[7] SWGDRUG Mass Spectral Library, www.swgdrug.org. (accessed December 2021)
The article has been published in German as:
- Wenn Leichen auf Gerichtsmediziner treffen: Ein letztes Urteil,
Nadine Theofel, Sonja Roscher, Stefan Scholtis, Michael Tsokos,
Chem. unserer Zeit 2019, 53, 40–49.
https://doi.org/10.1002/ciuz.201800862
and was translated by Caroll Pohl-Ferry.
When Corpses Meet Forensic Pathologists – Part 2
Forensic toxicology case history: Choose your pills wisely
When Corpses Meet Forensic Pathologists – Part 3
Case history 2: When hallucinogens become deadly
See similar articles published in ChemistryViews


this was helpful, cheers mate <3