Forensic sciences are a highly diverse field. Forensic toxicology, for example, can play an important role. In the first part, we looked at what forensic medicine is and what happens in the autopsy room. In this and the following part, we provide a look behind the scenes at two representative case reports that illustrate the different approaches followed in the field of forensic toxicology. In this article, we will look at how forensic pathologists track down which substances might have caused death and at the case example of a young woman.
4. Which Substances Contributed to the Poisoning?
To judge if the identified substances contributed to the death, the next step is to determine the concentration of the drug or medication in the blood. In many forensic toxicology labs, blood from the femoral vein is used for this because it remains unchanged for a long time and the concentration found will come closest to that at the time of death. The concentrations of active metabolites (metabolic products) are also determined. This requires preparation of the sample for analysis.
Unlike depictions in television series, pure blood cannot be injected. Sample preparation is carried out either by protein precipitation with an organic solvent such as methanol or acetonitrile, or by solid-phase extraction with a mixed-mode reversed phase. Both sample preparation methods have advantages and disadvantages. Precipitation with methanol or acetonitrile does not exclude any substances from the analysis. However, the complexity of the chromatograms is maintained due to the incompletely removed matrix.
In contrast, solid-phase extraction is a much more complex sample preparation procedure than precipitation. In this process, the matrix is separated out much better, so that the chromatograms are less complex. However, it is possible to lose analytes in the sample preparation procedure. This has to be checked on a case-by-case basis. Please read more details about the procedures in the literature [8].
4.1. Quantitative Determination of Medications
For the quantitative determination of medications, a liquid chromatograph (LC) is coupled to a diode array detector (DAD). This coupling is an extremely accurate measuring technique, features a broad linear range, and is very cost-effective. I was successfully used many times in the past [9] because many medications absorb light in the ultraviolet range and have an easily detectable concentration in the µg/mL range in cases of poisoning.
However, this requires that the analyte in question (the toxin) is chromatographically separated from the other analytes in the sample. This is only possible if finely tuned chromatographic conditions are used. In practice, various isocratic (solvent composition remains constant) conditions are tried and then the conditions that lead to the “purest” UV spectrum for the peak (the toxin) are chosen. The “purity” is a good gauge of this.
4.2. Quantitative Determination of Drugs and Low-Dose Medications
 In contrast, drugs and low-dose medications are quantified with a significantly more sensitive procedure, in which various LC/MSMS configurations are used (see Infobox 3 in Part 1). For this, an appropriate 2H- or 13C-labeled internal standard is added to the sample at the beginning of the analytical process to compensate for losses that occur during extraction and measurement. In the end, these labeled substances have similar physicochemical properties as the corresponding unlabeled analyte (the toxin). The measurement is subsequently carried out in either the MRM (multiple reaction monitoring) mode or by means of the highly resolved mass of the quasi-molecular ion.
In contrast, drugs and low-dose medications are quantified with a significantly more sensitive procedure, in which various LC/MSMS configurations are used (see Infobox 3 in Part 1). For this, an appropriate 2H- or 13C-labeled internal standard is added to the sample at the beginning of the analytical process to compensate for losses that occur during extraction and measurement. In the end, these labeled substances have similar physicochemical properties as the corresponding unlabeled analyte (the toxin). The measurement is subsequently carried out in either the MRM (multiple reaction monitoring) mode or by means of the highly resolved mass of the quasi-molecular ion.
In principle, it would also be possible to obtain an MRM measurement with a triple quadrupole mass spectrometer coupled to a gas chromatograph. However, the LC/MSMS coupling avoids extensive sample preparation, as the sample does not need to be derivatized. It is only necessary to precipitate the protein and dilute the sample.
The determined concentration can then be evaluated using a substance list [10] and secondary literature, such as the “Baselt” [11], which cite the concentrations of many toxins in many deaths. In addition, the wealth of experience of experts is not insignificant in reaching an assessment. Even so, it should not be forgotten that every case is unique. The case history, autopsy result, degree of habituation, age, and alleged pre-existing conditions must all be considered. These data must not contradict each other.
5. Choose Your Pills Wisely
 Two cases that occurred in Berlin in 2016 are presented below. Both cases are unique and demonstrate how variable the approaches can be in the field of forensic toxicology in forensic medicine.
Two cases that occurred in Berlin in 2016 are presented below. Both cases are unique and demonstrate how variable the approaches can be in the field of forensic toxicology in forensic medicine.
In the first case history, a classic narcotic, 3,4-methylenedioxy-N-methylamphetamine (MDMA, see Infoboxes 1 and 4 and Fig. 5), played a fatal role; in the second case, it was a new psychoactive substance, 4-bromo-2,5-dimethoxyphenylethylamine (2C-B).
 |
|
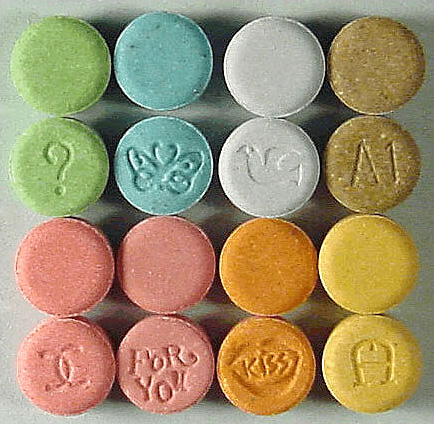
Figure 5. Ecstasy pills. |
5.1. Case History: A Young Woman Underestimates the Effect of Ecstasy Tablets
5.1.1. Background
A 27-year-old woman (height: 162 cm, weight: 76 kg, BMI: 29) was out with fellow students in Berlin and partied with them until the early hours of the morning. According to witness statements, narcotics were consumed over the course of the evening. In the end, all the students returned to their vacation rental to eat and drink some more. After a few hours, one of the students noticed first respiratory distress and then unconsciousness in the decedent. At the hospital, the victim was treated for five more days, until respiratory failure due to lack of oxygen and a cerebral edema were diagnosed.
A toxicological urine screening at the hospital came back positive for drugs. A witness found a square, 10×10 mm tablet stamped with “Fortissio” and the “Nespresso” logo. This tablet contained an elevated dose of MDMA (for more information, see Infoboxes 1 and 4). In the end, the police assumed a case of intoxication with narcotics. There was no indication that the amphetamine derivative had been given to the young woman by a third party.
5.1.2. Alcohol Analysis
Because the deceased was in the hospital for a week, ethanol (<0.1 ‰) could no longer be detected in her femoral vein blood. It had already been completely degraded.
5.1.3. Systematic Toxicological analysis
In a first step, the sample from the corpse was tested immunochemically for prevalent drugs and medications. It was then analyzed by GC/MS because not all drugs can be found with immunological group tests and the poisoning can only be identified by this means. In the context of immunochemical analysis, no abnormalities can be determined within the groups tested (for an overview, see Fig. 3 in Part 1).
The GC/MS screening detected the hospital medications primidone and propofol, as well as the metabolite phenobarbital. These substances are not detected by routine tests. Propofol is in the narcotics family and primidone is an anticonvulsive (drug against seizures). Phenobarbital is a metabolite of primidone.
5.1.4. Quantitative Analysis
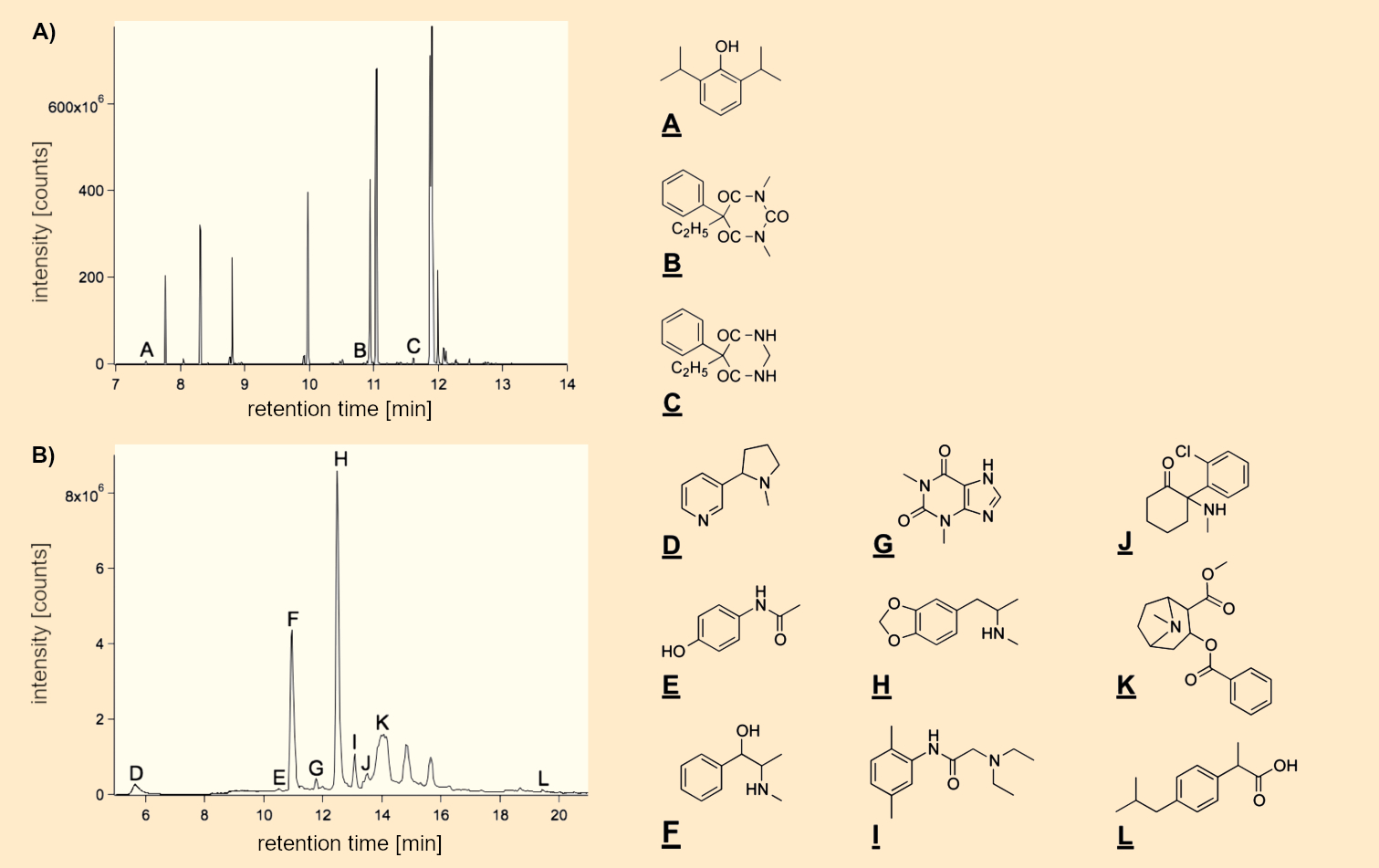
The concentrations of the medications in the femoral vein blood (see Fig. 6A) were below the therapeutic range [propofol: 0.7 µg/mL (therapeutic: 2–8 µg/mL), primidone: 2 µg/mL (therapeutic: 4–12 µg/mL), so a medical error could not be assumed.
 |
|
Figure 6. Representative ion chromatograms of A) femoral vein blood and B) hair of the deceased. The blood sample was processed via a C18 mixed-mode phase and subsequently methylated with trimethylsulfonium hydroxide. In contrast, for LC/MSMS analysis, the hair sample was extracted for 3 h at 50 °C and centrifuged. The supernatant liquid was then analyzed. GC/MS analysis: A: propofol, B: demethylated phenobarbital, C: primidone; LC/MS analysis: D: nicotine, E: paracetamol, F: pseudoephedrine, G: theophylline, H: MDMA, I: lidocaine, J: ketamine, K: cocaine, L: ibuprofen. |
5.1.5. Hair Analysis
Because the victim was very young and had partied in a club in Berlin, and because at least one “NESPRESSO” tablet was found at the club the next day, the next step of the inquiry was to pursue whether drugs could be detected in the hair of the deceased.
According to the literature, it is still possible to very reliably detect the parent substance and lipophilic metabolites in hair after several weeks or months. Because the deceased had long hair, three representative segments were chosen for analysis: the proximal, medial, and distal ranges. This made it possible to draw conclusions about the victim’s consumption of drugs about 6, 12, and 18 months ago.
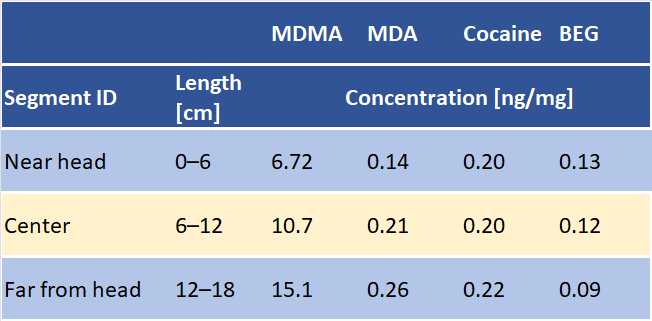
MDMA and cocaine, as well as their primary metabolic products (see Fig. 6B) were found in the hair of the deceased, which raises the suspicion that she had used drugs in the past. Surprisingly, the concentration of MDMA increased in going from the segment close to the head (consumption in the last 6 months) to the segment farthest from the head (consumption in the last 18 months). In contrast, the concentrations of cocaine remained unchanged throughout the entire strand of hair (see Tab. 1). Hair analysis cannot rule out that the substances found were transferred to the hair through sweat or sebum. After all, the deceased fought for her life for several days.
|
Table 1. Quantitative detection of MDMA, MDA (metabolite of MDMA), cocaine, and BEG (metabolite of cocaine) in the hair. |
 |
Hair analysis [12] is an established procedure in living individuals. However, the interpretation of hair analysis in corpses is not so simple. Factors such as sweat, the structure of the hair, frequency of washing, and the consumption and application of various hair products have an enormous influence on the concentration and thus on the quantitative detection of the target substances in hair. Moshoff and Madea compiled many hair analyses [13], but the interpretation of hair analyses requires great experience, and the interpretations must be carried out with great care and consideration of the case history.
5.1.6. Evaluation
The chemical toxicological tests show no indication of an acute deadly intoxication or excessive consumption of medical substances. According to the police investigation file, the deceased had consumed drugs. The consumption of drugs shortly before the time of death could not be detected due to the length of the patient’s survival time in the hospital. At the time of death, the drugs were long gone from the body of the deceased.
To consider previous drug consumption, additional hair from the head was thus examined. Various narcotics were detected (see Fig. 6 and Tab. 1), which leads to the conclusion that there was previous consumption of these substances. The high concentration of MDMA in the hair (usual dose of MDMA + MDA for one ecstasy tablet per month: 4 ng/mg [14]) leads to the conclusion of MDMA intoxication. Finally, it cannot be determined if this was caused by the consumption of multiple tablets or one overdosed tablet like the “NESPRESSO” tablet (for a warning about “NESPRESSO” tablets, see [15]).
References
[8] T. Stimpfl et al., Recommendations on Sample Preparation of Biological Specimens for Systematic Toxicological Analysis, www.tiaft.org. (accessed December 22, 2021)
[9] F. Pragst et al., Systematic toxicological analysis by high-performance liquid chromatography with diode array detection (HPLC-DAD), Clin. Chem. Lab. Med. 2004, 42, 1325–1340. https://doi.org/10.1515/CCLM.2004.251
[10] M. Schulz et al., Therapeutic and toxic blood concentrations of nearly 1,000 drugs and other xenobiotics, Crit. Care 2012, 16, R136. https://doi.org/10.1186/cc11441
[11] R. C. Baselt, Disposition of Toxic Drugs and Chemicals in Man, Biomedical Publications, Seal Beach, CA, USA, 2020. ISBN: 9780578577494
[12] F. Scheufler, Haare im Fokus der forensischen Analytik (in German), Chem. unserer Zeit 2018, 52, 26−33. https://doi.org/10.1002/ciuz.201700760
[13] B. Madea, F. Mußhoff, Haaranalytik Technik und Interpretation in Medizin und Recht (in German). Deutscher Ärzte-Verlag, Köln. 2004. ISBN: 3-7691-0437-4
[14] G. A. Cooper et al., Hair Analysis: Self-Reported Use of “Speed” and “Ecstasy” Compared with Laboratory Findings, J. Forensic Sci. 2000, 45, 400–406.
[15] Vorsicht, hochdosierte XTC-Pille „Nespresso“ mit 191,8 mg MDMA*HCL (in German), mindzone.info. (accessed December 22, 2021)
The article has been published in German as:
- Wenn Leichen auf Gerichtsmediziner treffen: Ein letztes Urteil,
Nadine Theofel, Sonja Roscher, Stefan Scholtis, Michael Tsokos,
Chem. unserer Zeit 2019, 53, 40–49.
https://doi.org/10.1002/ciuz.201800862
and was translated by Caroll Pohl-Ferry.
When Corpses Meet Forensic Pathologists – Part 1
A look behind the scenes at two cases that illustrate the different approaches used in forensic toxicology
When Corpses Meet Forensic Pathologists – Part 3
Case history 2: When hallucinogens become deadly
See similar articles published in ChemistryViews




